Don’t Suffer in Silence
Get Relief from Piles in a Daycare!
Laser Piles Treatment in Bangalore (Hemorrhoids)

If you are searching for the most advanced laser piles treatment in Bangalore, Hari Laser Clinics offers modern, patient-friendly solutions.
Piles — also known as hemorrhoids — affect millions of people worldwide. Globally, about 50% to 66% of people will experience hemorrhoids at some point in their lives (Wikipedia – Hemorrhoids). In India too, studies show that a significant percentage of adults over the age of 30 report symptoms such as bleeding, pain, or swelling.
In earlier times, surgery for piles was dreaded due to pain, stitches, and long recovery. But today, advanced laser techniques have made treatment far more comfortable. At Hari Laser Clinics, we provide laser piles treatment in Bangalore, a modern solution designed to minimize pain, reduce hospital stay, and speed up healing.
Our procedures are performed as daycare surgeries, meaning most patients return home the same day and resume normal activities within 2–3 days. Treatment is led by Dr. Varun Kumar J, MBBS, DNB, FIAGES – General & GI Surgeon, ensuring safe, personalized, and effective care.
What Are Piles?
Piles, medically known as hemorrhoids, are swollen and inflamed veins in the rectum or anus that develop due to increased pressure in the lower rectal area. This condition can cause discomfort, itching, bleeding, or pain, depending on its severity.
There are two main types of piles based on their location:
Internal Piles: Found inside the rectum, usually painless but often cause bleeding during bowel movements.
External Piles: Located under the skin around the anus, typically painful, itchy, and may form clots (thrombosed piles) that cause swelling and severe discomfort.
While piles are not life-threatening, untreated cases can lead to chronic pain, infections, and complications such as anal fissures or abscesses.
Modern medical approaches — including laser piles treatment in Bangalore — offer a safe, painless, and minimally invasive solution with faster healing and minimal downtime compared to conventional surgery.
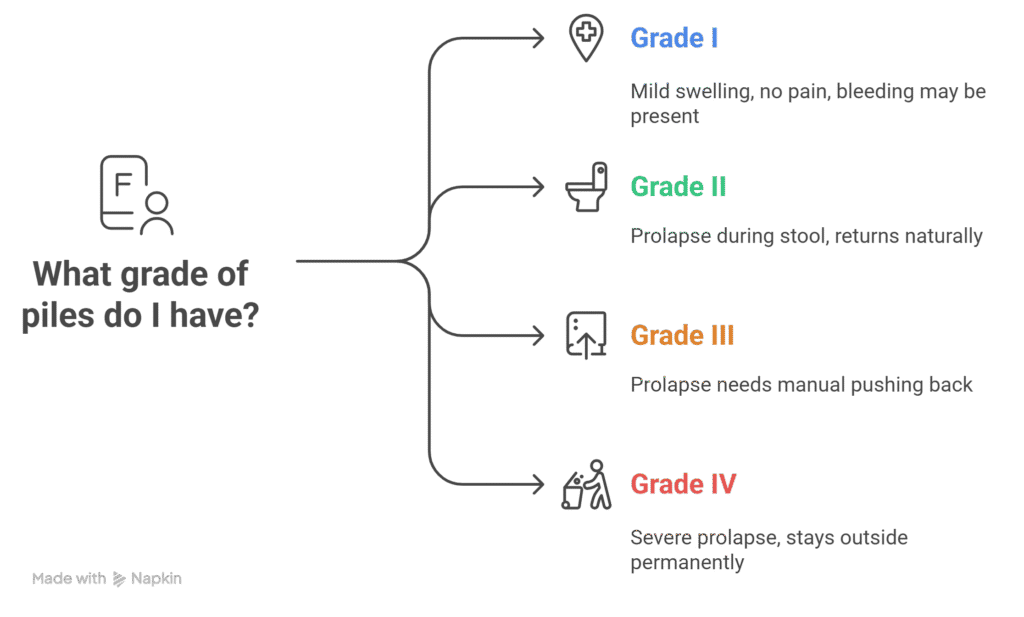
Grades of Piles
Doctors classify piles into four grades based on severity:
Grade I: Mild swelling inside the rectum. Usually no pain but bleeding may be present.
Grade II: Piles prolapse during stool but return inside naturally.
Grade III: Prolapsed piles need manual pushing back inside.
Grade IV: Severe prolapse stays outside permanently and can form clots or cause infections.
Grades I–II may improve with medicines and lifestyle adjustments. Grades III–IV generally require advanced procedures like laser piles treatment in Bangalore for permanent relief.
Patients Often Ask:
Can Grade I piles heal without surgery?
Yes. Grade I piles can often be managed with dietary changes, medicines, and lifestyle improvements. Surgery or laser treatment is considered if symptoms persist.
Symptoms of Piles
Piles (also called hemorrhoids) often start with mild discomfort but can progress into more noticeable symptoms if left untreated. Recognizing these early signs helps ensure faster recovery and minimally invasive treatment such as laser piles treatment in Bangalore.
Bleeding during bowel movements: Bright red blood on toilet paper or in the stool is one of the first signs of piles.
Pain or discomfort: Sharp or throbbing pain, especially while sitting, passing stool, or after prolonged standing.
Itching and irritation: Persistent itch or burning sensation around the anus caused by swelling and moisture.
Swelling or lump near the anus: A small, tender lump that may indicate external piles.
Mucus discharge or prolapse: In advanced grades, the swollen veins may protrude outside the anus, leading to discomfort and hygiene issues.
Ignoring these symptoms can lead to chronic pain, infection, or clot formation. Early diagnosis by an experienced piles doctor in Bangalore ensures effective management through medication or laser piles surgery.
If you notice bleeding, swelling, or persistent discomfort, consult a specialist for piles treatment in Bangalore for early evaluation and safe, long-term relief.
Freedom from Piles in a Day
Don’t Suffer Anymore!!

Book your Appointment!
Causes of Piles
Piles occur when the veins around the anus or rectum experience excessive pressure, leading to inflammation and swelling. Understanding the root causes of piles helps prevent recurrence and ensures early management through diet, lifestyle changes, or advanced procedures like laser piles treatment in Bangalore.
Common Causes
Chronic Constipation or Straining: Repeated straining during bowel movements increases pressure on rectal veins, causing them to enlarge and bulge.
Low-Fiber Diet: Insufficient fibre intake hardens stool, making passing it more difficult and painful.
Sedentary Lifestyle: Prolonged sitting, especially during office work or driving, restricts blood circulation in the anal region.
Pregnancy: Added pressure on the pelvic veins increases the risk of piles in women.
Obesity: Excess body weight exerts constant pressure on rectal veins.
Genetic Predisposition: Family history or weaker vein walls can make piles more likely.
Aging & Chronic Coughing: Weakened connective tissues and repeated abdominal strain contribute over time.
Making small adjustments — such as eating a fibre-rich diet, staying hydrated, and exercising regularly — can help prevent piles naturally. If symptoms persist, consult a specialist for piles surgery in Bangalore for long-term relief.
Patients Often Ask:
Does pregnancy always cause piles?
No. Pregnancy increases the risk, but not all women develop piles. Good hydration, fiber intake, and regular check-ups lower the risk.
Risk Factors
While piles can affect anyone, certain conditions and habits significantly raise the risk. Recognizing these piles risk factors helps in timely prevention and treatment.
Major Risk Factors
Age Over 40: Natural weakening of tissues increases susceptibility.
Prolonged Sitting: Office workers, drivers, and sedentary individuals are more prone.
Heavy Lifting: Frequent strain during workouts or manual labor elevates abdominal pressure.
Poor Hydration: Inadequate water intake leads to constipation and harder stools.
Chronic Diarrhoea: Repeated bowel movements cause irritation and vein damage.
Postpartum Period: Hormonal changes and strain during delivery raise risk in women.
While not all risk factors can be avoided, early lifestyle correction and medical consultation can help control symptoms and prevent recurrence.
What Is Laser Piles Treatment?
Laser piles treatment is a modern, bloodless, and minimally invasive procedure that uses focused laser energy to treat hemorrhoids with precision and safety.
Here’s what makes it one of the best laser piles treatment options in Bangalore:
Key Highlights
Minimally invasive & stitch-free – No cuts, no sutures, and minimal tissue damage.
Painless recovery – Laser seals the swollen veins, reducing pain, swelling, and bleeding.
Quick procedure – Performed under local or spinal anaesthesia; usually a same-day discharge.
Faster healing – Most patients resume normal activities within a few days.
Very low recurrence – Laser precisely targets only affected tissue, preventing future flare-ups.
Safe for all grades of piles – Effective for both internal and external hemorrhoids.
Better cosmetic outcome – No open wounds or scarring compared to conventional surgery.
Compared to traditional piles surgery, Hari Laser Clinics, Bangalore ensures minimal discomfort, quicker recovery, and long-term relief for patients seeking painless, effective treatment.
Laser vs Open Surgery – Comparison Table
| Feature | Laser Surgery | Open Surgery |
|---|---|---|
| Pain | Minimal | Moderate – Severe |
| Bleeding | Very less | High |
| Hospital Stay | Daycare / Same day | 2 – 3 days |
| Recovery Time | 2 – 3 days | 2 – 3 weeks |
| Recurrence Rate | Very low | Higher |
| Stitches | None | Yes |
| Infection Risk | Minimal | High |
Benefits of Laser Piles Treatment
Laser piles treatment offers a safe, painless, and highly effective solution for hemorrhoids. Compared to conventional surgery, it ensures faster healing, minimal discomfort, and better long-term results.
Painless and stitch-free procedure – Minimal discomfort during and after treatment.
Same-day discharge – Performed as a quick daycare procedure; no hospital stay needed.
Rapid recovery – Most patients resume normal activities within 2–3 days.
Minimal bleeding and tissue damage – Laser seals the affected veins precisely.
Lower recurrence risk – Targets only diseased tissue, reducing chances of relapse.
Infection-free healing – Laser cauterization prevents wound contamination.
Better cosmetic outcome – No external scars or sutures.
Safe for all age groups – Ideal for working adults, seniors, and postpartum women.
Covered by major health insurance plans – Affordable and accessible care.
These advantages make Hari Laser Clinics, Bangalore the preferred choice among patients seeking fast, painless, and permanent relief from hemorrhoids.
Patients Often Ask:
Why is laser treatment preferred over open surgery?
Because it is less painful, recovery is faster, and recurrence rates are much lower.
Types of Treatment Options Available
Treatment for piles depends on the grade, severity, and symptoms of the condition. At Hari Laser Clinics, our specialists, led by Dr. Varun Kumar J, follow a personalized and step-wise approach — beginning with conservative therapies and moving to advanced laser solutions only when required.
High-fibre diet, hydration, stool softeners, and topical ointments help relieve early-stage piles.
Sitz baths (warm-water soaks) reduce pain and swelling.
Ideal for mild cases; focuses on prevention and symptom control.
Note: These methods ease discomfort but do not permanently remove hemorrhoids.
When piles persist or prolapse, minimally invasive procedures are recommended for faster, long-term relief:
Laser Piles Surgery (Preferred): Uses precision laser energy to shrink or seal hemorrhoidal tissue. Painless, bloodless, and allows same-day discharge.
Stapler (ZSR) Surgery: Effective for large, prolapsed piles. A circular stapling device repositions and seals tissue simultaneously, ensuring quick recovery.
Rubber Band Ligation: A small elastic band cuts off blood supply to the hemorrhoid, causing it to dry and fall off naturally.
Infrared Coagulation (IRC): Uses focused infrared light to shrink smaller internal hemorrhoids with minimal discomfort.
Reserved for Grade IV piles or complex recurrent cases.
Involves surgical removal of hemorrhoidal tissue under anaesthesia.
Effective but requires stitches and a longer healing period.
Recommended only when laser or stapler options are not feasible.
At Hari Laser Clinics, our team ensures that every patient receives the safest, least invasive, and most effective piles treatment in Bangalore — ensuring quick recovery, minimal pain, and long-term relief.
Comparison Table – Treatment Options by Grade
| Grade | First Line Treatment | Next Step | Advanced Option |
|---|---|---|---|
| I | Lifestyle + Diet | Medicine / Ointments | — |
| II | Medicines + Ligation | Laser Surgery | Stapler (rare) |
| III | Supportive Care | Laser Surgery | Stapler Surgery |
| IV | Supportive Only | Laser Surgery | Open Surgery (if severe) |
Pre-Care Instructions
Preparing well before your laser piles treatment in Bangalore ensures a safe procedure, smooth experience, and faster recovery. Follow these essential pre-care guidelines as advised by your doctor:
Eat light, easily digestible meals the day before surgery to keep your digestive system clear.
Avoid smoking and alcohol for at least 48 hours prior, as they can affect anaesthesia and healing.
Share your complete medical history — including medications, supplements, and allergies — to help your doctor plan the safest approach.
Stay well-hydrated and get adequate rest for optimal body function before the procedure.
Arrange for a companion if you’re undergoing sedation or anaesthesia to assist you post-procedure.
Following these pre-care steps helps reduce surgical risks and promotes faster recovery after your piles surgery.
Post-Care Instructions After Laser Piles Treatment
Proper aftercare following laser piles treatment in Bangalore ensures faster recovery, minimizes complications, and promotes long-term relief. Patients should follow these steps carefully:
Follow a high-fiber diet including fruits, vegetables, and whole grains to maintain soft stools and reduce strain.
Stay hydrated by drinking plenty of water to prevent constipation.
Take warm sitz baths to relieve pain, itching, and promote healing in the anal region.
Avoid straining during bowel movements to protect the treated area.
Refrain from heavy lifting or strenuous activity for at least a week to prevent recurrence or complications.
Take prescribed medications (painkillers, ointments, or stool softeners) as directed.
Attend follow-up appointments to monitor healing and ensure optimal results.
Patients Often Ask:
When can I return to work after laser piles surgery?
Most patients resume routine activities in 2–3 days and recover fully within a week.
Recovery Timeline
Day 0: Same-day discharge after surgery.
Day 2–3: Resume routine tasks and office work.
Week 1: Return to heavy work, exercise, and strenuous activities.
Prevention of Piles
Adopting healthy lifestyle habits is key to preventing piles and reducing the risk of recurrence after treatment. Here are expert-recommended steps:
Eat a high-fiber diet: Include fruits, vegetables, and whole grains to keep stools soft and prevent straining.
Stay hydrated: Drink at least 8–10 glasses of water daily to support smooth bowel movements.
Exercise regularly: Even 30 minutes of walking or light physical activity improves digestion and blood circulation in the rectal area.
Avoid prolonged sitting: Take short breaks if you work long hours at a desk or drive frequently.
Respond promptly to bowel urges: Delaying bowel movements increases pressure on rectal veins.
Maintain a healthy weight: Reduces excess pressure on the anal and rectal veins, lowering the risk of piles.
Prevention is always better than cure. Incorporating these habits can significantly lower the chances of recurrence and support faster healing after laser piles treatment in Bangalore.
About the Author - Dr. Varun Kumar J

MBBS, DNB (General Surgery), FIAGES, FMAS
Dr. Varun Kumar J,
MBBS, DNB (General Surgery), FIAGES, FMAS
General & Laparoscopic Surgeon | Laser & Varicose Vein Specialist
Dr. Varun Kumar J is an experienced Laparoscopic and Laser Surgeon in Bangalore with over 14 years of expertise in minimally invasive surgery. He specializes in piles, fissure, fistula, varicose veins, and hernia treatments using advanced laser techniques.
Known for his compassionate care and precision, Dr. Varun ensures every procedure is safe, simple, and stress-free for his patients.
Experience: 14+ Years
Hospitals: Medfine Hospital & Hari Laser Clinics, Bangalore.
Why Choose us for Piles Treatment?
Advanced Laser Techniques
We use USFDA-approved laser treatments for painless and scar-free piles removal. These minimally invasive techniques ensure faster recovery and reduced pain compared to traditional methods.
Expert Care by Dr. Varun Kumar J
Dr. Varun Kumar J ensures each treatment is personalized for the patient’s needs, providing comprehensive care for long-term relief.
Quick Recovery
Most patients can resume normal activities within 24 hours due to our non-invasive procedures and fast healing.
Post-Surgery Support
Our dedicated team offers post-treatment guidance, including follow-ups and recovery tips to promote optimal healing.
Commonly Asked Questions
What patients search for piles treatment?
Patients search for a variety of information related to piles (hemorrhoid) treatment, focusing on symptom relief, treatment options from home remedies to surgery, prevention methods, and guidance on which doctor to consult.
What are the common symptoms of piles, and how can they be managed?
Piles can cause bleeding during bowel movements, pain, itching, burning sensation, swelling near the anus, mucus discharge, or a feeling of incomplete bowel emptying. Early symptom management includes improving diet, hydration, bowel habits, and consulting a doctor before the condition worsens.
How can piles symptoms be relieved at home?
Mild piles symptoms may improve with warm sitz baths, adequate water intake, fiber-rich foods, and avoiding straining while passing stools. Home remedies can offer short-term relief, but persistent symptoms should always be medically evaluated.
Do over-the-counter (OTC) medicines cure piles permanently?
OTC creams, ointments, and suppositories may temporarily reduce pain, itching, or swelling. However, they do not treat the root cause of piles. Recurrent symptoms often indicate the need for advanced medical treatment.
What lifestyle changes help prevent piles from worsening?
Healthy lifestyle habits play a key role in piles management. Avoid straining, do not sit on the toilet for long periods, stay physically active, maintain a healthy weight, and follow a consistent bowel routine to reduce pressure on rectal veins.
Which foods should be avoided during piles?
Patients with piles should avoid spicy foods, fried foods, junk food, alcohol, excessive caffeine, and refined flour products. These foods can worsen constipation and irritation, leading to increased pain and bleeding.
What are the best foods to eat for piles relief?
High-fibre foods such as fruits, vegetables, whole grains, oats, lentils, beans, and seeds help soften stools and reduce strain. Drinking enough water is equally important for effective relief.
What is the ideal diet plan for piles patients?
An ideal piles diet includes high fiber, good hydration, minimal processed foods, and regular meal timing. A consistent diet helps control symptoms and lowers the risk of recurrence.
What are minimally invasive treatment options for piles?
Minimally invasive treatments manage piles with less pain and faster recovery. These include laser piles treatment, rubber band ligation, and infrared coagulation. Among these, laser treatment offers higher precision and comfort.
What is the most advanced and modern treatment for piles?
Laser piles treatment is a modern, minimally invasive procedure that treats piles using focused laser energy. It causes minimal tissue damage, less bleeding, reduced pain, and quicker recovery compared to traditional surgery.
What tests are done to diagnose piles accurately?
Diagnosis may involve a physical examination, digital rectal exam, and procedures such as anoscopy or sigmoidoscopy. These tests help determine the grade of piles and rule out other causes of rectal bleeding.
How do bowel habits affect piles?
Poor bowel habits like straining, delaying stools, or prolonged toilet sitting increase pressure on rectal veins. Correct bowel habits significantly improve symptoms and reduce the chance of recurrence.
Which doctor should I consult for piles treatment?
A proctologist or an experienced general surgeon is the right specialist for piles evaluation and treatment. Early consultation helps avoid complications and ensures faster recovery.
I have itching and burning around the anus. Is it always piles?
Not always. Itching and burning may be caused by piles, anal fissures, infections, or skin conditions. A medical examination is necessary to identify the exact cause and start appropriate treatment.
What are the common risk factors for piles?
Risk factors include chronic constipation, prolonged sitting, obesity, pregnancy, low-fiber diet, lack of physical activity, heavy lifting, and advancing age. Managing these factors lowers the risk of piles.
How does laser treatment work for piles?
Laser treatment uses controlled laser energy to shrink or remove piles tissue while sealing blood vessels. This results in minimal bleeding, less post-procedure pain, and faster healing.
Does rectal bleeding always mean piles?
No. While piles are a common cause, rectal bleeding can also occur due to fissures, infections, polyps, or other conditions. Any bleeding should be evaluated by a doctor.
What should piles patients strictly avoid?
Piles patients should avoid straining during bowel movements, sitting for long hours, heavy lifting, ignoring symptoms, and unhealthy eating habits that worsen constipation.
What is the best sleeping position for piles patients?
Sleeping on the side, particularly the left side, helps reduce pressure on rectal veins and improves circulation, providing better comfort during recovery.
Which exercises are safe and beneficial for piles patients?
Low-impact exercises such as walking, yoga, stretching, and breathing exercises help improve digestion and bowel function. Heavy weightlifting and high-impact workouts should be avoided during active symptoms.
Is piles a lifelong disease?
Piles are not always permanent. With proper treatment, lifestyle changes, and advanced options like laser piles treatment, many patients achieve long-term relief without recurrence.
When should piles treatment not be delayed?
If symptoms such as bleeding, pain, prolapse, or discomfort persist despite home care, early medical treatment is essential to prevent complications and improve quality of life.
Why choose laser piles treatment for faster recovery?
Laser piles treatment offers minimal pain, no stitches, reduced hospital stay, and quicker return to daily activities, making it a preferred option for many patients.
Common Patient Searches Related to Piles (Hemorrhoids)
Patients experiencing piles often search online for clear, reliable information before consulting a doctor. These searches usually fall into four key areas:
Symptom Management and Immediate Relief
The first concern for most patients is reducing pain, swelling, and discomfort. Common searches focus on:
Home remedies for piles such as sitz baths, ice packs, and natural soothing agents like witch hazel or aloe vera.
Over-the-counter (OTC) piles treatments, including creams and ointments containing hydrocortisone or lidocaine, suppositories, and mild pain relievers like acetaminophen or ibuprofen.
Lifestyle and dietary changes such as increasing water intake and eating high-fiber foods (fruits, vegetables, whole grains) to soften stools and reduce straining during bowel movements.
Treatment Options: Non-Surgical and Surgical
When home remedies do not provide adequate relief, patients actively research medical treatments for piles:
Minimally invasive piles treatments, including rubber band ligation, sclerotherapy (injection therapy), infrared coagulation, and laser procedures—often comparing pain levels, effectiveness, and recovery time.
Surgical treatment for piles, such as hemorrhoidectomy and stapled hemorrhoidopexy, especially for advanced or recurrent cases.
Laser treatment for piles, which attracts high interest due to benefits like minimal pain, faster recovery, no stitches, and shorter hospital stays compared to traditional surgery.
Diagnosis and Doctor Consultation
Many patients are unsure about the severity of their condition and seek guidance on medical evaluation:
Which doctor to consult for piles, including whether to visit a general physician, gastroenterologist, or proctologist/colorectal surgeon.
When to seek medical help for piles, particularly in cases of persistent bleeding, severe pain, prolapsed hemorrhoids, or painful lumps that do not improve with home care.
Diagnostic tests for piles, such as physical examination, digital rectal exam, anoscopy, or colonoscopy, and what to expect during these procedures.
Prevention and Long-Term Management of Piles
Patients also look for long-term solutions to prevent recurrence and maintain digestive health:
Diet plans for piles prevention, including high-fiber foods to eat (leafy greens, whole grains) and foods to avoid (spicy foods, processed foods, alcohol, caffeine).
Healthy bowel habits, such as avoiding prolonged sitting on the toilet, not straining during bowel movements, staying physically active, and maintaining proper hydration.
